Dublin’s Most Reviewed Physio Clinic
Before You Book Your Appointment, Here's Just a Handful of Our 10,000+ Patients Success Stories to Put Your Mind at Ease
Your First Appointment. What To Expect
Tired of Living With Pain? We Can Help

Not sure who to ask?
Not sure what to do next?
Not sure who can help?
Please fill out the form below and chat with one of our team members about your right next step
Meet The Team

Joseph Boland
Management

Craig O'Grady
Personal Trainer

Daire Lynch
Physiotherapist

Eoin Mc Kearney
Physiotherapist

Roisin O Brien
Physiotherapist
Dublin’s Most Reviewed Physio Clinic - 1,000+ Reviews
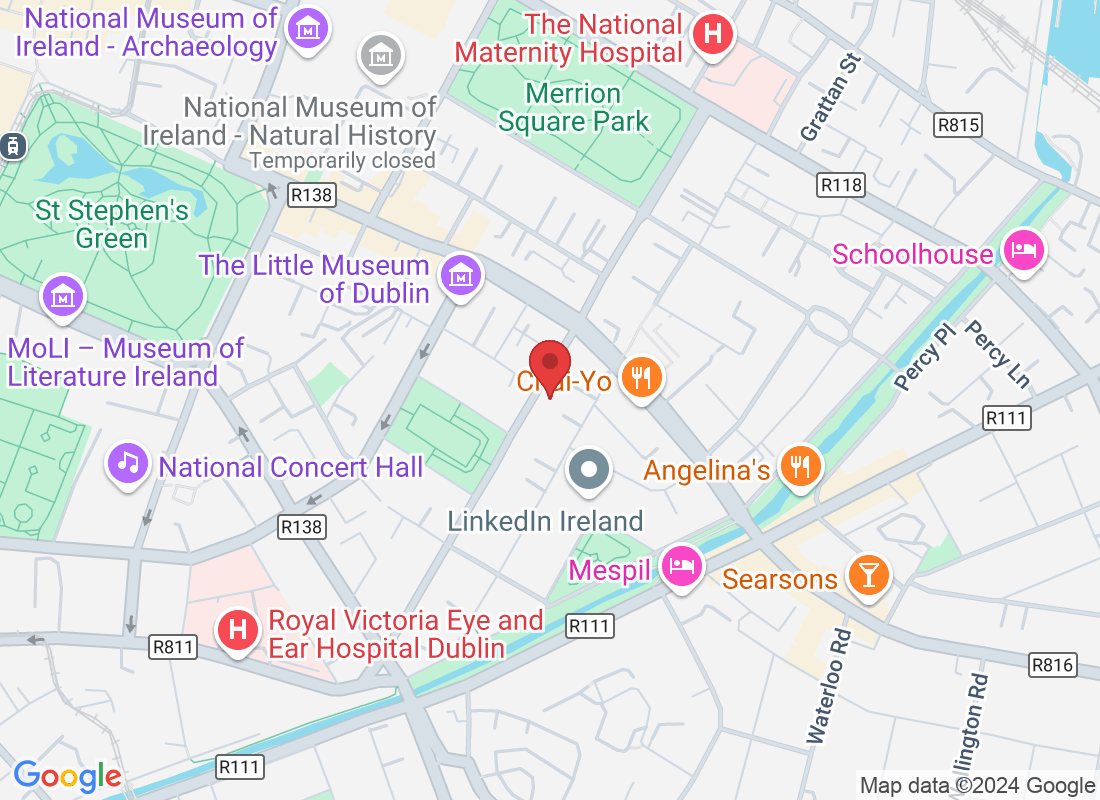
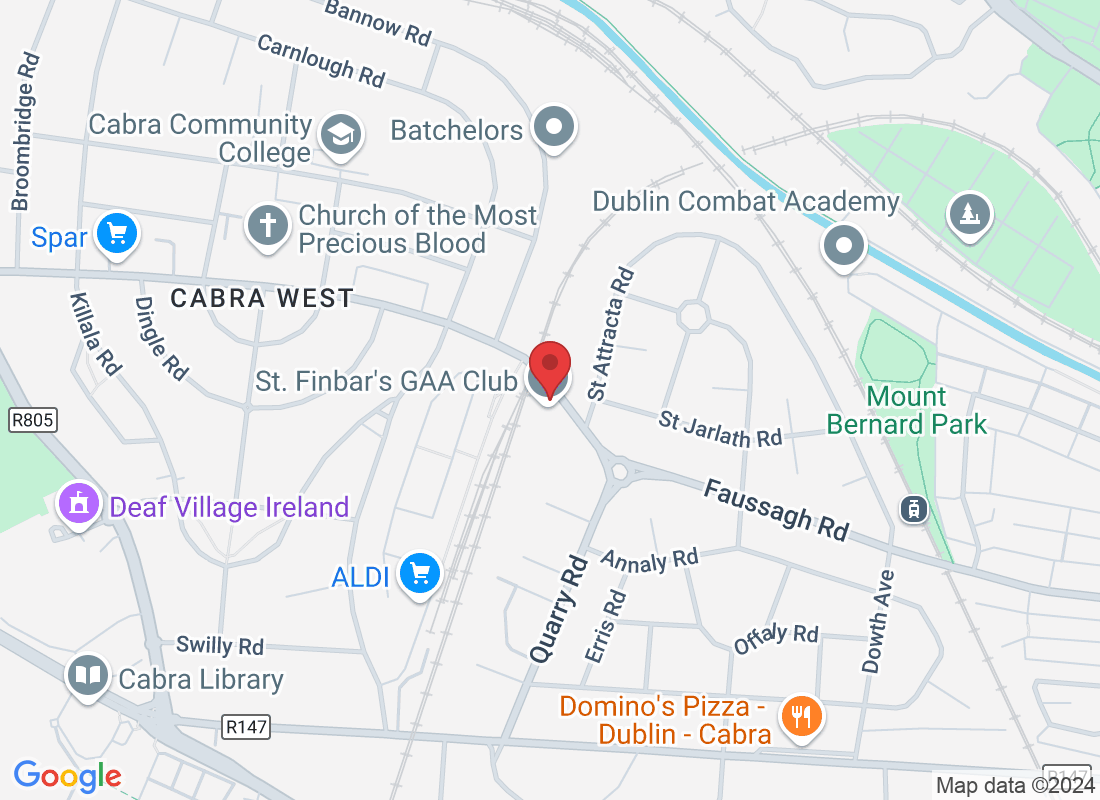
Dublin 2 & Dublin 7
Still Feeling A Little Confused About Your Condition And Don't Know What To Do?
#1 Option (👍 most popular)

#2 Option - WhatsApp Us

#3 Option - Book Appointment


From Consultation to Treatment
What to Expect at Your First Physio Visit
We're excited to see you at your appointment! We want to make sure you feel comfortable and well-informed, so don't hesitate to ask us any questions about our treatments, our clinic, or even our payment options. Our goal is to help you get back to living your life free of pain, so let's work together to make that happen!
Discuss your fitness and health goals
Complete assessment
Discover your options
Start a custom treatment plan


Here's Why Over People Choose Sports Physio Ireland

Specialised Expertise: Our clinic offers specialised care from highly-trained physiotherapists in various fields like sports rehab and chronic pain management.
Comprehensive Approach: We provide holistic treatment plans combining manual therapy, exercises, and cutting-edge technology for a well-rounded approach.
Cutting-Edge Facilities: Equipped with state-of-the-art facilities and advanced equipment to support patients' recovery.
Proven Track Record: Our clinic's reputation is built on successful patient outcomes and positive feedback, fostering a supportive environment for rehabilitation.
We've Answered the Most Common Questions New Patients Often Ask...
What conditions do you treat?
Physiotherapists treat a wide range of conditions such as sports injuries, joint pain, back pain, post-operative rehabilitation, neurological conditions, and more.
What should I expect during the initial assessment?
The initial assessment involves discussing your medical history, current symptoms, performing physical tests, and developing a treatment plan tailored to your needs.
How many sessions will I need?
The number of sessions varies based on individual needs and the nature of the condition. It will be discussed during the assessment, and the treatment plan will be adjusted accordingly.
What types of treatments do you offer?
Physiotherapy treatments may include exercises, manual therapy, ultrasound, heat/cold therapy, electrical stimulation, and education on posture and ergonomics.
Will I be given exercises to do at home?
Yes, home exercises are often an integral part of treatment. They help speed up recovery and maintain progress between sessions.
How long will it take to see improvement?
Improvement timelines vary depending on the condition, individual factors, and adherence to the treatment plan. Consistency and following the therapist's advice can expedite progress.
What if I have pain during or after treatment?
It's normal to experience some discomfort during or after certain treatments or exercises. However, if pain is severe or persistent, it's essential to inform the physiotherapist for adjustments to the plan.
Do I need a referral from a doctor?
In many cases, you can directly access physiotherapy without a doctor's referral. However, some insurance plans or specific conditions might require a referral, so it's best to check beforehand.
How can I prevent this injury from recurring?
Physiotherapists provide guidance on injury prevention strategies, including exercises, lifestyle modifications, and ergonomic advice to reduce the risk of re-injury.
What should I wear to my sessions?
Wear comfortable clothing that allows easy movement and access to the area being treated. Sometimes, you might be asked to change into specific attire, so it's good to inquire beforehand.
Please note that these FAQs provide general information and should not replace personalised advice from a qualified healthcare professional. It is important to consult with a trusted physiotherapist to assess your individual case and determine the most suitable treatment plan for your condition.
Still Confused? Don't Worry! Download One of Our Helpful Information Packs to Get Unstuck
Low Back Pain
Unlock fast solutions for ending back pain and stiffness naturally

Shoulder Pain
Discover how to naturally ease neck and shoulder tension

Knee Pain
Quick ways to walk for longer with less knee pain
Dublin 2
Opening Hours
Monday: 7:00am - 8:00pm
Tuesday: 7:00am - 8:00pm
Wednesday: 7:00am - 8:00pm
Thursday: 7:00am - 8:00pm
Friday: 7:00am - 8:00pm
Saturday: 7:00am - 3:00pm
Sunday: Closed
Dublin 7
Opening Hours
Monday: 11:00 am - 7:00 pm
Tuesday: Closed
Wednesday: 5:00pm - 8:00pm
Thursday: 7:00 am - 3:00 pm
Friday: 7:00 am - 3:00 pm
Saturday: Closed
Sunday: Closed
First Floor, Naomh Fionnbarra GAA Club - Physiotherapy, Faussagh Ave, Cabra East, Dublin 7, D07 TFT2